Ali, Mohammed, MBChB, MSc, MBA, RSPH, Global Health - Cardiometabolic disease epidemiology, implementation sciences, global health
Alonso, Alvaro, MD, PhD, RSPH, Epidemiology - CVD Epidemiology, cardiac arrhythmias, neurodegenerative diseases
Bremner, J. Douglas, MD, Emory SOM, Psychiatry - Mental health, neurobiology of stress
Cooper, Hannah, PhD, RSPH, Behavioral Sciences - Social determinants of health, minority health, health inequities, community health, geospatial, multilevel analysis
Dickert, Neal, MD, PhD , Emory SOM, Medicine (Cardiology) - Cardiovascular medicine, bioethics, public health ethics
Druss, Ben, MD, MPH, RSPH, Health Policy - Mental health, health services, health policy
Dunbar, Sandra, RN, PhD, Emory SON - Health behaviors, psychosocial factors, intervention research
Gazmararian, Julie, PhD, RSPH, Epidemiology - Social determinants of health, health behaviors, nutrition, obesity, health policy, community health, implementation sciences
Johnson, Dayna, MPH, PhD, RSPH, Epidemiology - Sleep epidemiology, health disparities, social determinants of health, CVD epidemiology
Jones, Dean, PhD, Emory SOM, Pulmonary - Metabolism, nutrition, metabolomics, redox mechanisms
Kegler, Michelle, PhD, RSPH, Behavioral Sciences - Health behaviors, obesity, community-based participatory research, implementation sciences
Komro, Kelli RSPH, Behavioral Sciences & Epidemiology - Health promotion interventions through community and policy change; cluster-randomized trials to reduce high-risk behaviors and health disparities
Kulshreshtha, Ambar, MD, PhD, FAHA, FAAFP, RSPH, Epidemiology, Emory SOM, Medicine (Family Medicine) - health disparities and prevention of heart disease and Alzheimer’s dementia.
Lash, Timothy, MPH, DSc, RSPH, Epidemiology - Epidemiology methods, molecular epidemiology
Lewis, Tené, PhD, RSPH, Epidemiology - Social determinants of health, CVD epidemiology, minority health, health inequities, women’s health, psychosocial factors
Lim, S. Sam, MD, Emory SOM, Rheumatology - Minority health, chronic inflammatory/autoimmune disorders
Lopez-Cepero, Andrea, PhD, RSPH, Epidemiology - population health researcher focusing on the prevention of cardiometabolic diseases among Latinx populations, particularly obesity and type 2 diabetes.
Winkler, Megan, PhD RSPH, Behavioral Sciences - population health scientist and former clinician focusing on health disparities, health promotion, obesity prevention, public health policy, and social determinants of health
Mehta, Puja, MD, FACC, FAHA, Emory SOM, Medicine (Cardiology) - women and cardiovascular disease, and diagnosis and treatment of coronary microvascular dysfunction and ischemic heart disease.
Narayan, Venkat, MD, MPH, RSPH, Global Health - Cardiometabolic disease epidemiology, diabetes, global health policy
Ofotokun, Ighovwerha, MD, MSc, Emory SOM, Infectious Diseases & RSPH, Epidemiology - HIV co-morbidities including CVD
Patel, Shivani A., MPH, PhD,, RSPH, Global Health and Epidemiology - the role of ethnic background, contextual factors (such as historical undernutrition, urbanization, migration, geography), and early life disadvantage in influencing cardio-metabolic disease profiles.
Pearce, Brad, PhD, RSPH, Epidemiology - role of genetics, infections, immune interactions and behavioral factors in the etiology of complex disorders, including autism, schizophrenia, and preterm birth.
Quyyumi, Arshed, MD, Emory SOM, Medicine (Cardiology) - Vascular biology, vascular function, cardiovascular health disparities
Searles, Charles, MD, Emory SOM, Medicine (Cardiology) - Vascular biology, molecular biology
Shah, Amit, MD, MSCR, RSPH, Epidemiology - Cardiovascular epidemiology, psychosocial factors, mind-body relations
Stein, Aryeh, PhD, RSPH, Global Health - Nutrition, global health, cardiovascular epidemiology, bioethics
Suglia, Shakira, PhD, RSPH, Epidemiology - Cardiovascular epidemiology, Latino health, health disparities, psychosocial factors, children/adolescent health
Sun, Yan, PhD, RSPH, Epidemiology - Genetics, epigenetics
Taylor, Herman, MD, Morehouse SOM - Social determinants of health, racial disparities, interventions and implementation sciences
Vaccarino, Viola, MD, PhD, RSPH, Epidemiology - CVD epidemiology, women’s health, psychosocial factors
Waller, Lance, PhD, RSPH, Biostat+Bioinformatics - Biostatistics/bioinformatics, geospatial analysis
Wilson, Peter, MD, Emory SOM, Medicine (Cardiology) - Cardiometabolic epidemiology, genetics


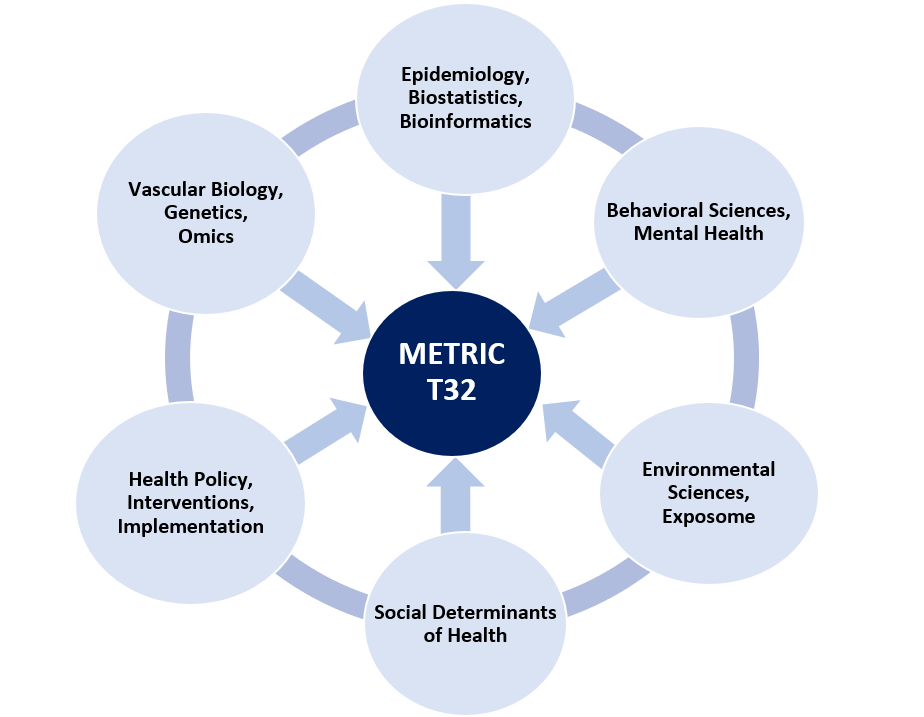 The METRIC T32 training grant is housed in the Department of Epidemiology, and draws faculty with diverse expertise and at various career stages from all Emory Schools (School of Public Health, School of Medicine and School of Nursing) and Morehouse School of Medicine. The Program Director is Dr. Viola Vaccarino in the Department of Epidemiology. The Program Co-Director is Dr. Arshed Quyyumi in the Department of Medicine.
The METRIC T32 training grant is housed in the Department of Epidemiology, and draws faculty with diverse expertise and at various career stages from all Emory Schools (School of Public Health, School of Medicine and School of Nursing) and Morehouse School of Medicine. The Program Director is Dr. Viola Vaccarino in the Department of Epidemiology. The Program Co-Director is Dr. Arshed Quyyumi in the Department of Medicine.